One of the biggest obstacles is Gram-negative bacteria’s protective outer barrier, which is extremely difficult to penetrate.
There’s no lack of chemicals that can kill bacteria. One of the main reasons there have been so few new antibiotics developed in recent decades – apart from a poor return on investment – is that researchers have run out of ideas on how to outwit the protective mechanisms of Gram-negative bacteria.
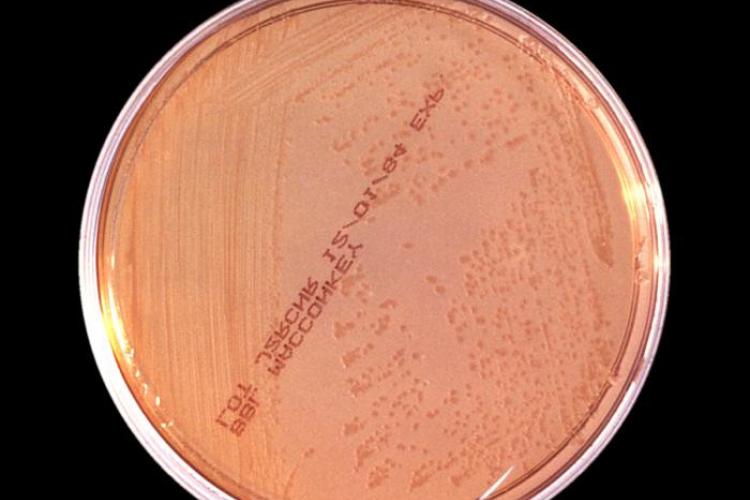
Gram-negative and Gram-positive describe types of bacteria based on the structure of their cell walls. It refers to how they appear when they come into contact with violet-coloured dye in the laboratory. Gram-positive bacteria will stay violet-coloured because their cell wall retains the dye; while Gram-negative cell walls don’t. It’s a quick way to reveal which antibiotic is likely to treat your infection.
Gram-negative bacteria don’t retain the violet staining because the external layer that’s typically found in Gram positive bacteria is partially substituted by an extra outer membrane. This makes them less permeable to chemical compounds as well as antibiotics. They are behind some of the most serious infections in humans (like pneumonia, salmonella, plague…), and multidrug resistance is rising. Gram-negative bacteria are the subject of many of IMI’s antimicrobial research projects.
Proteins, porins, receptors
The task for researchers is to figure out how new drugs can be made to outmanoeuvre this membrane and get them inside the bacterial cell. The outer membrane provides an extra layer of protection, but it also allows the material that the bacteria need to sustain life – basically, its ‘food’ – to pass through unhindered. The complex structure of the membrane, and the way it carries out this food delivery service, are not yet fully understood. What we do know is that the membrane is studded with two types of proteins through which molecules can cross the outer membrane. These proteins are called porins and receptors, which are like pores. Proteins’ role in keeping bacteria out of reach of antibiotics, and their potential as drug targets, is being studied by scientists hoping to break the impasse in antibiotic research.
The IMI TRANSLOCATION project carried out intensive studies of these porins and receptors. The project team were able to describe many features of the protective cell membranes that control the access and expulsion of compounds from bacteria, down to the atomic level. Their research revealed the detailed structures of 40 different proteins involved in drug transport.
Permeability scoring method
TRANSLOCATION produced a scoring function to predict a drug’s permeability, which is basically a loose set of rules about drug likelihood to pass through porins, and sensitive methods to detect how much drug ends up inside the cell. They showed how receptors could be hijacked to allow entry of 'Trojan Horse' antibiotics, designed to resemble food. The project studied efflux pumps, another protection method used by Gram-negative bacteria to pump drugs back out of the cell once they make it past the two membranes.
Being able to predict the likelihood of a potential antibiotic getting into the bacterial cell will help scientists figure out which chemicals are worthy of further study, hopefully speeding up research and eventually, bringing new antibiotics to the market.
Read more
New antibiotics won't stop AMR. Luckily, there are other things we can try. by Pierre Meulien, IMI Director.
A very promising antibiotic just started clinical trials
Technology, not instinct, should guide antibiotic prescribing
"AMR is an area that needs fresh ideas" - interview with Isabelle Bekeredjian Ding
