COMBACTE’s networks are helping overcome a persistent bottleneck in testing drugs against AMR – the relatively small numbers of cases in individual hospitals
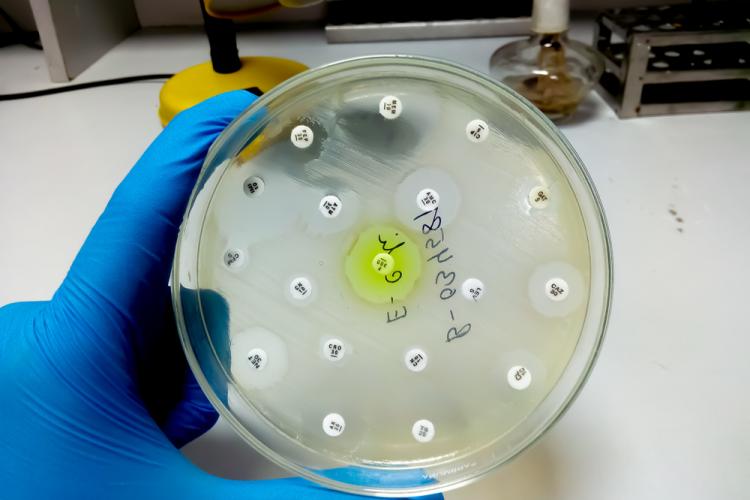
Antimicrobial resistance (AMR) is a huge, looming problem. Carrying out clinical trials of new treatments is very difficult, and one of the reasons is that the absolute number of infections caused by AMR in a single hospital is actually quite low, meaning individual sites don’t generally have enough cases to be able to properly evaluate a treatment. Bacterial infections also need to be treated as soon as they are diagnosed, meaning that the window for testing treatment options is small.
As part of the COMBACTE project, a network of prepared and equipped clinical sites connected to diagnostic laboratories, called CLIN-Net and LAB-Net, were launched in 2014 to help overcome this problem. The network provides strong infrastructure to run clinical trials of new antimicrobial agents across multiple sites, and is the only one of its kind in the world, putting Europe in a leadership position in clinical research into infectious diseases.
Once up and running, the network was immediately put to use, allowing pharma partners in the project to test novel antibacterials faster, more effectively and more economically. As additional support, EPI-Net was established in 2015 to meet the need for a comprehensive source of published data related to epidemiological aspects of AMR that healthcare professionals, pharmaceutical companies and the lay public can find easily.
What happens long-term
The networks built under COMBACTE will gradually become a new entity called the European Clinical Research Alliance for Infectious Diseases (ECRAID). It will be a separate legal entity led by the key players of the COMBACTE networks, among others.
ECRAID will set up several perpetual observational studies (POS). The disease areas for which POSs are currently being established are infections picked up via ventilation in intensive care, as well as complicated urinary tract infections and yeast infections in new-borns, among others. A platform trial for patients with severe community-acquired (i.e. not in the hospital) pneumonia is already fully operational in ECRAID (see the REMAP-CAP study).
The clinical sites participating in these studies are trained and adequately resourced. Prepared to implement new studies, they will enroll patients on an ongoing basis, and are supported by well-trained diagnostic laboratories. The ECRAID network is available for all investigators (academic researchers and private partners) that want to execute large clinical studies, offering both operational support and scientific expertise. Pharmaceutical companies and medical technology companies, large and small, can benefit from ‘on-demand’, direct, single-point-of-access to a large, international high-quality clinical network, while governmental organisations (policy makers, funders, regulators) can have fast and efficient access to rigorous evidence and data to support public health measures in the case of acute infectious diseases outbreaks.
COVID19 collaborations
Although CLIN-Net and LAB-Net were originally conceived to respond to the threat of AMR, they were involved in the PREPARE project, which focusses rapid scientific response to infectious disease threats. When COVID19 emerged, the network was immediately used for finding suitable clinical sites in hospitals and primary care for COVID19-related studies, as part of, for instance, the RECOVER project, one of the number of EU-funded projects launched in response to the pandemic.
“One of the many lessons learned from this pandemic is that operational networks are needed for a rapid scientific clinical response,” says Prof. Marc Bonten, coordinator of COMBACTE and the H2020-funded ECRAID-Base, from the University Medical Center Utrecht in the Netherlands
“With a new disease with high morbidity and mortality, evidence on treatment effectiveness needs to be delivered within weeks or months, and not years.”
“This includes both clinical interventions, meaning antimicrobials, vaccines, diagnostics, treatment regimens etc. as well as public health interventions like quarantine measures, lockdowns, hygiene measures, physical distancing, face masks etc. Therefore, we strongly recommend making such networks an integral part of pandemic preparedness. In the inter-pandemic periods such a network can be used to evaluate many aspects of diagnosing, treating and preventing non-pandemic infections,” he adds.
“That will maintain the operational capacity and with regular trainings for a rapid response, the network can be rapidly activated and adapted to the scientific needs in the initial stage of a future pandemic.”
Related
For research projects to leave a legacy, long-term vision is vital
Drug safety academic programme expands to North America
A one-stop-shop for disease-specific human stem cells allows scientists to focus on research
